Alcoholism linked to lack of intestinal bacteria | ScienceNordic

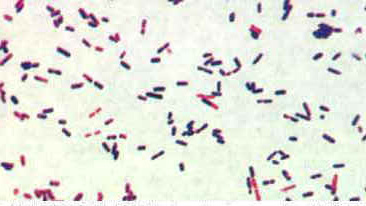
It
could be that some alcoholics have a particularly hard time quitting
the alcohol because they have fewer intestinal bacteria than other
people. (Photo:
Shutterstock)
A new study suggests that bacteria in the gut may play a role in alcohol addiction and the risk of relapse after rehab.
"Our
results provides strong evidence that alcohol addiction is not only in
the brain, but that it in some cases can be associated with an imbalance
in the intestinal flora,” said Professor Fredrik Bäckhed from the
University of Gothenburg during a guest lecture at Novo Nordisk
Foundation Center for Basic Metabolic Research at Copenhagen University.
Some alcoholics have fewer intestinal bacteria
In the study, which was
recently published in the journal PNAS, Bäckhed and his colleagues from Belgium and Sweden have analysed the intestinal bacteria composition of 60 alcoholics.
The 60 alcoholics in the study had an equal use of alcohol.
After
the test participants had spent 19 days in rehab it became apparent to
the scientists that there was a big difference in how well the
participants recovered: their well-being and risk of relapse was
connected to their gut flora.
26 out of the 60 alcoholics suffered
from leaky gut syndrome and generally had a low amount of intestinal
bacteria -- specially their levels of
Faecalibacterium prausnitzii,
which is known for its anti-inflammatory properties, were detected as
unusually low. The leaky gut syndrome is linked to inflammation of the
gut and diseases like Crohn disease.
After 19 days without alcohol
the 26 test subjects still scored high on tests that measuered
depression, anxiety, and alcohol cravings. There was in fact not much
difference from before they went to rehab.
In comparison, the
remaining 34 subjects with normal gut flora were recovering much better,
scoring low on depression, anxiety, and alcohol cravings. In fact,
their scores decreased to levels comparable with the control group who
didn't have a drinking problem.
On the basis of these results the
scientists concluded that intestinal flora is connected to the
likelihood of relapse after sobering up in rehab.
Bäckhed hopes that the study will lead to new treatment possibilities for alcoholics where the intestinal flora is considered.
Our results strongly suggest that alcohol addiction is not only a problem which starts in the brain
Professor Bäckhed
"It
appears that some alcoholics may need a different treatment than
others. The study has an interesting treatment potential,“ he said.
Professor: The study does not prove a connection
Professor Ove
Schaffalitzky, head of research at the department of gastroenterology,
University of Southern Denmark, is not entirely convinced that the new
study shows a link between intestinal bacterial flora and alcohol
addiction. He was not involved in the study, but has read it.
“The study does indeed show a correlation, however, this doesn't necessarily prove anything," said Schaffalitzky.
Even
though there is some overlap it does not prove that there is a
connection between intestinal flora and increased alcohol addiction, he
says.
“There can be other explanatory factors which the study does
not account for. It may be that the test subjects have a special
drinking pattern or diet, have other illnesses, have a special gut or
something else. There are many uncertain points in the hypothesis,” said
Schaffalitzky.
The brain-gut connection is still not clear
Although Bäckhed is
certain that there is a link between the bacteria in the gut and alcohol
addiction, he also stresses that there is a need for more studies,
before we can understand the exact relation.
“It's the first time
we have shown that there is a correlation between alcohol craving and
bacterial gut composition. Previously studies with mice have produced
similar results," said Bäckhed. "However, we still don't know how the
connection between the gut and the brain works."