Pathogenic Clostridia, including Botulism and Tetanus (page 1)
(This chapter has 4 pages)

Clostridium botulinum
Clostridia
The genus
Clostridium consists of relatively large, Gram-positive,
rod-shaped
bacteria in the Phylum Firmicutes
(Clostridia is actually a
Class in the Phylum).
All species form endospores
and have a strictly fermentative type of
metabolism.
Most clostridia will not grow under aerobic conditions and vegetative
cells
are killed by exposure to O2, but their spores are able to
survive long
periods of exposure to air.
The clostridia are ancient organisms that live in virtually all of
the
anaerobic habitats of nature where organic compounds are present,
including
soils, aquatic sediments and the intestinal tracts of animals.
Clostridia are able to ferment a wide variety of organic compounds.
They produce end products such as butyric acid, acetic acid, butanol
and
acetone, and large amounts of gas (CO2 and H2)
during fermentation of
sugars.
A variety of foul smelling compounds are formed during the fermentation
of amino acids and fatty acids. The clostridia also produce a wide
variety
of extracellular enzymes to degrade large biological molecules (e.g.
proteins, lipids, collagen, cellulose, etc.) in the
environment
into fermentable components. Hence, the clostridia play an important
role
in nature in biodegradation and the carbon cycle. In anaerobic
clostridial
infections, these enzymes play a role in invasion and pathology.
Most of the clostridia are saprophytes, but a few are pathogenic for
humans, primarily Clostridium
perfringens, C. difficile, C. tetani and C. botulinum. Those that are pathogens
have primarily a saprophytic existence
in nature and, in a sense, are opportunistic pathogens. Clostridium
tetani and Clostridium botulinum produce the most potent
biological
toxins known to affect humans. As pathogens of tetanus and food-borne
botulism,
they owe their virulence almost entirely to their toxigenicity. Other
clostridia,
however, are highly invasive under certain circumstances.

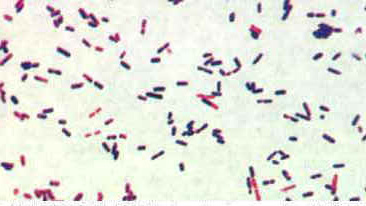
Stained pus from a mixed
anaerobic
infection. At least three different clostridia are apparent.
Clostridium perfringens

C. perfringens
Clostridium perfringens, which produces a huge array of
invasins
and exotoxins, causes wound and surgical infections that lead
to
gas
gangrene, in addition to severe uterine infections.
Clostridial
hemolysins and extracellular enzymes such as proteases, lipases,
collagenase
and hyaluronidase, contribute to the invasive process. Clostridium
perfringens
also produces an enterotoxin and is an important cause of food
poisoning.
Usually the organism is encountered in improperly sterilized (canned)
foods
in which endospores have germinated.
Food poisoning
Clostridium perfringens is classified into 5 types (A�E) on
the basis of its ability to produce one or more of the major lethal
toxins, alpha, beta, epsilon and iota (α, β, ε, and ι). Enterotoxin
(CPE)-producing (cpe+) C.
perfringens type A is reported continuously as one of the most
common food poisoning agents worldwide. An increasing number of reports
also implicate the organism in 5%�15% of antibiotic�associated
diarrhea (AAD) and sporadic diarrhea (SD) cases in humans, as well as
diarrhea cases in animals.
Most food poisoning strains studied carry cpe in their
chromosomes; isolates from AAD and SD cases bear cpe in a
plasmid. Why C. perfringens strains with cpe
located on chromosomes or plasmids cause different diseases has not
been satisfactorily explained. However, the relatively greater heat
resistance of the strains with chromosomally located cpe is a
plausible explanation for these strains' survival in cooked food, thus
causing instances of food poisonings. The presence of C.
perfringens strains with chromosomally located cpe in
1.4% of American retail food indicates that these strains have an
access to the food chain, although sources and routes of contamination
are unclear.
An explanation for the strong association between C. perfringens
strains with plasmid-located cpe and cases of AAD and SD
disease may be in vivo transfer of the cpe plasmid to C.
perfringens strains of the normal intestinal microbiota.
Thus, a small amount of ingested cpe+ C. perfringens
would act as an infectious agent and transfer the cpe plasmid
to cpe� C. perfringens strains of the normal
microbiota. Conjugative transfer of the cpe plasmid has been
demonstrated in vitro, but no data exist on horizontal gene
transfer of cpe in vivo, and whether cpe+ strains
that cause AAD and SD are resident in the gastrointestinal tract or
acquired before onset of the disease is unknown.
Case Study
Report of C. perfringens Food
Poisoning
Clostridium perfringens
is a common cause of outbreaks of foodborne illness in the United
States,
especially outbreaks in which cooked beef is the implicated source.
This
is a condensed version of an MMWR report that describes an outbreak of
C.
perfringens gastroenteritis following St. Patrick's Day meals of
corned
beef. The report typifies outbreaks of C. perfringens food
poisoning.
Report
On March 18, 1993, the
Cleveland
City Health Department received telephone calls from 15 persons who
became
ill after eating corned beef purchased from one delicatessen.
After
a local newspaper article publicized this problem, 156 persons
contacted
the health department to report onset of diarrheal illness within 48
hours
of eating food from the delicatessen on March 16 or March 17. Symptoms
included abdominal cramps (88%) and vomiting (13%); no persons were
hospitalized.
The median incubation period was 12 hours (range: 2-48 hours). Of the
156
persons reporting illness, 144 (92%) reported having eaten corned beef;
20 (13%), pickles; 12 (8%), potato salad; and 11 (7%), roast beef.
In anticipation of a large
demand
for corned beef on St. Patrick's Day (March 17), the delicatessen had
purchased
1400 pounds of raw, salt-cured product. Beginning March 12, portions of
the corned beef were boiled for 3 hours at the delicatessen, allowed to
cool at room temperature, and refrigerated. On March 16 and 17, the
portions
were removed from the refrigerator, held in a warmer at 120oF
(48.8oC), and sliced and served. Corned beef sandwiches also
were made for
catering
to several groups on March 17; these sandwiches were held at room
temperature
from 11 a.m. until they were eaten throughout the afternoon.
Cultures of two of three
samples
of leftover corned beef obtained from the delicatessen yielded greater
than or equal to 105 colonies of C. perfringens per
gram.
Following the outbreak,
public
health officials recommended to the delicatessen that meat not served
immediately
after cooking be divided into small pieces, placed in shallow pans and
chilled rapidly on ice before refrigerating, and that cooked meat be
reheated
immediately before serving to an internal temperature of greater than
or
equal to 165oF (74 C).
Analysis
C. perfringens is a
ubiquitous,
anaerobic, Gram-positive, spore-forming bacillus and a frequent
contaminant
of meat and poultry.
C. perfringens food poisoning is characterized
by onset of abdominal cramps and diarrhea 8-16 hours after eating
contaminated
meat or poultry. By sporulating, this organism can survive high
temperatures
during initial cooking; the spores germinate during cooling of the
food,
and vegetative forms of the organism multiply if the food is
subsequently
held at temperatures of 60-125oF (16-52oC). If
served without
adequate
reheating, live vegetative forms of C. perfringens may be
ingested.
The bacteria then elaborate the enterotoxin that causes the
characteristic
symptoms of diarrhea and abdominal cramping.
Laboratory confirmation of C.
perfringens foodborne outbreaks requires quantitative cultures of
implicated
food or stool from ill persons. This outbreak was confirmed by the
recovery
of greater than or equal to 105 organisms per gram of
epidemiologically
implicated food. An alternate criterion is that cultures of stool
samples
from persons affected yield greater than or equal to 106
colonies
per gram. Stool cultures were not done in this outbreak.
Serotyping
is not useful for confirming C. perfringens outbreaks and, in
general,
is not available.
Corned beef is a popular
ethnic
dish that is commonly served to celebrate St. Patrick's Day. The errors
in preparation of the corned beef in this outbreak were typical of
those
associated with previously reported foodborne outbreaks of C.
perfringens. Improper
holding temperatures are a contributing factor in most C.
perfringens
outbreaks
reported to CDC. To avoid illness caused by this
organism, food should be eaten while still hot or reheated to an
internal
temperature of greater than or equal to 165oF (74oC)
before serving.
Gas gangrene
Gas gangrene generally occurs at the site of
trauma or a recent surgical wound. The onset of gas gangrene is sudden
and dramatic. About a third of cases occur on their own. Patients who
develop this disease in this manner often have underlying blood vessel
disease (atherosclerosis or hardening of the arteries), diabetes, or
colon cancer.
Clostridium perfringens
produces many
different toxins, four of
which
(alpha, beta, epsilon, iota) can cause potentially deadly syndromes.
The toxins cause damage to tissues, blood cells, and blood vessels.
Gas gangrene is marked by a high fever, brownish pus, gas
bubbles under the skin, skin discoloration, and a foul odor. It is the
rarest form of gangrene, and only 1,000 to 3,000 cases occur in the
United States each year. It can be fatal
if not treated immediately.
Clostridium perfringens,
Gram Stain. Most clostridia are renowned for staining "Gram-variable".