download video: mp4

Find out more about Gideon's high fibre diet on the links below
http://www.med.monash.edu.au/cecs/gastro/prebiotic/resources/video-gallery.html
http://www.med.monash.edu.au/cecs/gastro/prebiotic/resources/menu-planning.html
NARRATION
New discoveries about food are rocking the foundations of medicine and nutrition.
Professor Charles Mackay
I think this is one of the biggest developments in medical research. I really think we're encountering a revolution that maybe we can prevent diseases by simply changing our diet.
NARRATION
Last time on Catalyst, we learned about this paradigm-changing new research.
Dr Graham Phillips
The bottom line is the modern Western diet could be making us very sick, contributing to heart disease, diabetes, asthma, emphysema, multiple sclerosis, even autism, and the list goes on.
NARRATION
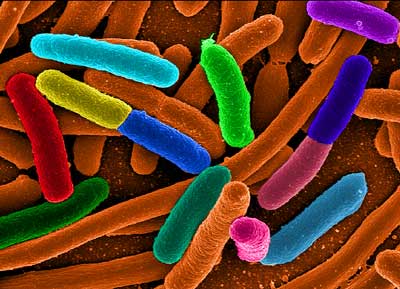
The reason for the revelation that a good diet is even more important than we thought is the discovery of the many trillions of new contributors to our health - the tiny good bacteria living in our guts.
Professor Stephen Simpson
It's a jungle in there. So there's a whole series of really fascinating biological interactions.
NARRATION
In a nutshell, if you eat a bad diet, you end up with bad gut bacteria, and these bugs send the wrong messages to the immune system. You could wind up sick.
Dr Graham Phillips
Now it's all very well to know that the modern Western diet is causing health problems - but what do you do about it? Well, that's what this second episode is all about and I can tell you now it's more than just changing the food you eat.
NARRATION
The reason the modern diet is so unhealthy is it's drifted far from the diets we evolved to eat.
Professor Stephen Simpson
So, settled agriculture saw a massive change in our diet and then, clearly, since the industrialisation of agriculture and the industrialisation of our food processing.
NARRATION
Professor Steve Simpson's been catching this healthy, unprocessed, pre-agriculture food since he was a kid.
Dr Graham Phillips
If we were kind of living in the Stone Age days, this would be how we'd be catching a meal, apart from we wouldn't have the fishing rods.
Professor Stephen Simpson
We wouldn't.
Dr Graham Phillips
We'd have to catch it with our hands. Was there a Stone Age diet, a single diet?
Professor Stephen Simpson
I think there were many Stone Age diets. So if you were by the coast, like here, obviously fish and shellfish would've been a big part of the diet.
NARRATION
But while there was no one caveman diet, there was one thing all these diets had in common - a lot of fibre. We saw this in the last episode with Africa's Stone Age Hadza people.
Professor Stephen Simpson
An average person in the West, man or woman, is consuming less than 20g a day of dietary fibre. And to put that into an evolutionary perspective, six-month- to one-year-old Hadza kids are eating 50g to 200g of fibre a day, every day, and they do this throughout life.
NARRATION
Now to understand why fibre is so important, try to imagine the magical universe within.
Professor Stephen Simpson
In the gut what you have is essentially a container with an entire world inside of it comprising hundreds if not thousands of species.
NARRATION
Just as the many species in this mangrove live together in harmony as an ecosystem, so do the species in our intestines. The gut ecosystem is called the microbiome and, like any ecosystem, it's tipped out of balance if the creatures in it don't get one of their fundamental foods. And for the bugs living here that's fibre. That's why the low-fibre food we eat these days can be so damaging. To see the effects of that, in the last episode we met Gideon - a young, fit gymnast. The two of us took a junk food challenge. After a typical high-fat, high-sugar feed, we had our bloods measured to see the effects. And Gideon was shocked to learn that while he was fit on the outside, on the inside, my much older body was performing better than his.
Professor Katherine Samaras
And, Gideon, essentially you needed two to three times as much insulin.
Gideon Cordover
This is a huge shock to me and quite nerve-racking.
NARRATION
My insulin levels were considerably lower than Gideon's. Indeed, he was on the road to diabetes. Why would this much younger man have such an unhealthy response? It became clear when we looked in his fridge. Not many health foods here.
Gideon Cordover
So I wake up in the morning, often I will eat what we had for dinner last night, tends to be kind of fast foods, so sometimes that'll be pizza. I'm a big fan of chicken burgers, so I eat a lot of fast food meals which often come with French fries, so big fan of French fries as well. Occasionally I eat at the pub - it will be usually a chicken burger, fries.
NARRATION
Almost all of Gideon's diet is processed food.
Professor Katherine Samaras
When we eat processed foods, it generates a whole lot of bacteria in our body that promotes inflammation, and these are the bad bacteria.
NARRATION
But the good news is give up the junk food and the inflammation reaction is turned down.
Professor Katherine Samaras
People who are lean and eat unprocessed food regularly have got all the good bacteria in their intestines.
NARRATION
So, we put a proposal to Gideon.
Dr Graham Phillips
Well, have we got an offer for you! How would you like us to put you on a healthy diet and see what changes it makes to your gut bacteria?
Gideon Cordover
A healthy diet?
Dr Graham Phillips
Carrot sticks, you know...
Gideon Cordover
A tasty diet?
Dr Graham Phillips
A tasty diet. It will be designed by a dietician.
Gideon Cordover
OK.
NARRATION
Monash University nutrition researcher Trish Veitch cooked up four weeks of healthy meals for Gideon.
Gideon Cordover
I'm nervous that I won't like the taste of some of the food that I'm gonna be eating, and I'm a bit nervous that I will feel hungry all the time because I'm used to eating huge quantities of fast food.
NARRATION
She also took him shopping, showing him the kind of food he should be buying.
Trish Veitch
These are persimmons. They're a source of really good prebiotic fibre.
Gideon Cordover
A whole new world of fruit and veg.
Trish Veitch
Indeed.
Gideon Cordover
The doctor said that this isn't, kind of, permanent damage that's been done, and so I guess it's given me more impetus to really take this diet seriously and actually make a good go of it.
Trish Veitch
Any of these beans are good for you.
Gideon Cordover
OK.
NARRATION
The plan is we'll look at Gideon's gut bacteria before and after his new diet, and we'll also remeasure his insulin response after four weeks of eating this healthy, but most importantly, high-fibre food.
Trish Veitch
Terrific.
Dr Graham Phillips
Alright. Yes, I reckon... can you do those zucchinis in thin strips?
NARRATION
Now, as it happens, I've been eating a fairly high-fibre diet lately.
Dr Graham Phillips
Yeah, that's perfect.
NARRATION
It wasn't my choice. Rather, I've developed allergies to dairy and wheat products - they give me sinus problems. And when you cut those out, you're left eating fairly high-fibre food.
Dr Graham Phillips
Now I eat about 50g of fibre a day, which is more than twice as much as the average Australian. I wonder what effect that's having on my gut bacteria.
NARRATION
Well, there's a way to find out. In Boulder, Colorado, is the headquarters of the American Gut Project. Here they collect samples of people's faeces from around the world, examining them to see just what kind of gut bacteria we're all carrying. Why are they doing it? I Skyped Rob Knight to find out.
Dr Graham Phillips
G'day, Rob.
Professor Rob Knight
Hey, Graham.
Dr Graham Phillips
What's the purpose of it? Why are you doing it?
Professor Rob Knight
Well, we're trying to find out what kinds of microbiomes are out there in the world. We're just beginning to find out how many kinds of communities there are even on one person.
NARRATION
By looking at samples from a wide variety of people, the goal is to eventually match particular microbiomes with particular health problems. Donating to the program is as simple as asking for a kit, and it can be fun.
Professor Rob Knight
You can also give it a gift to someone else, right? So if you have some family member, OK, you've just been dying all along to figure out exactly what kind of shit they're full of, now you can do that.
Dr Graham Phillips
Well, look, I always like to donate to worthy causes. This is kind of a bit odd, this one. But you'd accept a donation from me?
Professor Rob Knight
Absolutely.
NARRATION
Three days later, the kit turned up in the mail.
Dr Graham Phillips
Instructions. 'Collect a small amount of... biomass.' Way of putting it. 'More is not better.' OK. The things I do for science. But I guess it will be good to know what kind of gut bacteria I have.
Gideon Cordover
Hello, and welcome to day one of my video diary. For dinner, brown rice with lentils, which was a shock. And I had Greek yoghurt, Ryvita with hummus. Heaps and heaps of nuts. All kinds of nuts. Almonds and pistachios. I have experienced some mild discomfort, I would have to say, in terms of the old abdominal bloating.
NARRATION
Now, eating more fibre will improve your health. But there are other things you might be able to do, as well.
Dr Graham Phillips
Cheers.
Professor Matt Cooper
Cheers. That's quite sweet.
Dr Graham Phillips
Yeah. That's not bad.
Professor Matt Cooper
Shall we do shots?
Dr Graham Phillips
Shots sound perfect.
Professor Matt Cooper
Shots it is.
Dr Graham Phillips
Cheers.
Professor Matt Cooper
Down the hatch.
Dr Graham Phillips
Hoo!
Professor Matt Cooper
Ahh!
Dr Graham Phillips
Not as sweet. Ah!
NARRATION
This is no social drink. Professor Matt Cooper and I may be medicating ourselves. But they won't be adding these tipples to the wine list anytime soon. We're downing different kinds of vinegar because it could turn out to be a medicine.
Professor Matt Cooper
So the most important thing is to have a balanced diet and lots of high fibre. But we've also shown that with a lot of the studies we're doing in animals now that supplementing the diet by giving vinegar can actually stop things like asthma.
NARRATION
Treating asthma with vinegar? It seems remarkable. Unless of course you're into alternative health.
Dr Graham Phillips
The idea of using vinegar medicinally has been around for centuries.
Professor Matt Cooper
Oh, thousands of years, back to the Egyptian times, the Greek times. The beneficial effects of vinegars in society have been known for a long time. Even Italians - a lot of vinegar on salads, a lot of vinaigrette - they have very, very low incidences of inflammatory disease.
NARRATION
In fact, even the research on eating a good diet has an air of ancient wisdom about it.
Professor Charles Mackay
Hippocrates said 'Let thy food be thy medicine and thy medicine be thy food.' And we agree with that entirely.
NARRATION
The reason vinegar could be a medicine is because it contains acetate - that molecule we met in the first episode, the very one our good bacteria make.
Professor Matt Cooper
So we now know that acetate, which is very small and can get all around the body, can stop the immune system from overreacting.
NARRATION
By calming the immune system, it promotes good health. Matt Cooper developed asthma at about 18.
Professor Matt Cooper
I ended up taking a puffer twice a day and I was taking steroids two or three times a day. I had several incidents where I was really worried, I was almost gonna go to hospital, it was that bad. I was taking puff after puff, I could barely breathe.
Alessio
It hurts your chest a lot when you cough.
NARRATION
But now he's started eating more fibre and using liberal quantities of vinegar.
Professor Matt Cooper
I radically changed my diet. I dropped certain processed foods, I made sure it was brown rice, brown pasta, brown bread, bran in the morning and lots of fresh fruit and vegetables. And now I probably have one puff a year, if that.
Dr Graham Phillips
Really?
Professor Matt Cooper
Yeah.
Gideon Cordover
It's kind of going OK. I miss fast food. I really miss it.
NARRATION
Now, there are no proper clinical trials yet proving that vinegar can treat asthma in people, but there are results for mice. After showing she could reduce asthma in these animals by simply feeding them high-fibre food, Alison tried something else - she fed them acetate instead.
Dr Alison Thorburn
In fact, when we give acetate directly in the drinking water to the mice, that also suppressed their asthma.
NARRATION
So it seems incredible that simple stuff we splash on a salad may help treat a disease that plagues the Western world. And Alison's asthma story has taken yet another twist. She's fed high fibre to pregnant mice.
Dr Graham Phillips
Ah, there she is. So she's just given birth, has she?
Dr Alison Thorburn
Yeah, so she just gave birth yesterday morning.
Dr Graham Phillips
And so you've found something special about the diet in pregnant mice, right?
Dr Alison Thorburn
That's right. So she was actually on a high-fibre diet, and what we found was that when we gave pregnant mice the high-fibre diet and had a look at their offspring, their offspring didn't develop asthma. So they were protected against the development of asthma.
Dr Graham Phillips
So this is another thing for poor old mothers, is it? They can't drink, they can't smoke.
Dr Alison Thorburn
That's right.
Dr Graham Phillips
They've got to eat a high-fibre diet to reduce asthma.
Dr Alison Thorburn
Yep, yep.
NARRATION
Gut bacteria are tied up with a lot of other diseases, too. Take Professor Phil Hansbro's research on the devastating lung disease emphysema.
Professor Phil Hansbro
There are no current treatments that effectively suppress the disease and there's no treatments that stop the progression of disease.
NARRATION
Emphysema is a form of chronic obstructive pulmonary disorder, COPD.
Professor Phil Hansbro
A good way of explaining COPD is like taking a deep breath and then trying to take in a bit more breath and that last bit is the only breath that people with COPD can breathe in.
Dr Graham Phillips
Really? Let me try that. (Inhales deeply)
Professor Phil Hansbro
So another way of explaining it...
Dr Graham Phillips
Yeah, that's pretty awful.
Professor Phil Hansbro
Another way of explaining it is like trying to breathe through a straw.
NARRATION
The leading cause of emphysema in Australia is smoking. And remarkably, this activity, in mice at least, can push the gut microbiome out of balance.
Professor Phil Hansbro
So we think it not just affects the lung but there's systemic effects, and so that it affects the microbiome in the gut. We can show the changes in the microbiome that occur with cigarette smoke exposure and then we can also show which bacteria are altered, so which ones increase and which ones decrease.
NARRATION
And, excitingly, Phil's also found it may be possible to switch a bad emphysema biome for a more healthy one.
Professor Phil Hansbro
So mice are very good animals to study for this disease because when you co-house them they are actually coprophiles, and so they eat each other's poo.
NARRATION
Poo contains gut bacteria. Eat another's, and one acquires their bacteria.
Professor Phil Hansbro
So you can put mice in a box, some that are healthy and some that have COPD and emphysema, and they'd swap their microbiomes through eating each other's poo.
NARRATION
And the incredible result is mice that have emphysema get an improvement in symptoms after eating the poo of healthy mice. New gut bacteria have treated them.
Professor Phil Hansbro
It's really exciting stuff.
Dr Graham Phillips
So the good news is you've found a potential treatment for emphysema. The bad news is we have to eat each other's poo.
Professor Phil Hansbro
Well, that's quite correct. Although we can make it a lot more palatable by... and we call this 'transpoosion', which is a term that we're trying to bring into the literature.
NARRATION
Phil's transpoosion is, yep, a poo transplant. It involves taking faeces from a healthy person and putting them in the gut of someone suffering disease - hence providing them with new gut bacteria. Officially, it's known as a faecal transplant.
Dr Graham Phillips
I must say, this is one of the strangest procedures I've filmed as a science journalist. And, hey, I once filmed myself drinking my own urine, which I'd like to point out was properly filtered beforehand. But, you know, we may snigger and be a bit revolted by this procedure, but it could turn out to be a really important treatment.
NARRATION
No-one is yet doing faecal transplants in people for emphysema. But they are trialling the procedure for another debilitating disease thought to be connected to bad gut bacteria - ulcerative colitis. It's an inflammatory bowel disease and Anna has suffered it for more than half a decade.
Anna Demasi
So I was sick at about 22, so I'm 29 now, and I had really bad diarrhoea, you know, I couldn't control it, going to the toilet, you know, 30, 40 times a day. And I couldn't sleep, fevers, sore back. Those 30, 40 times a day was not food, it was mostly just blood and water.
Dr Graham Phillips
I mean, that must have had a huge impact on your life.
Anna Demasi
You can't go anywhere. You can't plan for trips, can't plan anything, can't even go to the shops to buy something.
NARRATION
This inflammatory bowel disease can be treated with powerful drugs but they can have terrible side effects.
Anna Demasi
My face would blow up like three times the size in a matter of days. I'd put 10, 15 kilos in a matter of a few weeks. And then the mental things, you'd get quite anxious and very aggressive. And you also couldn't sleep at night. So just a horrible, really horrible drug.
NARRATION
So a new treatment for the condition is being trialled at Sydney's St Vincent's Hospital - a faecal transplant.
Dr Graham Phillips
Now, it's a full medical procedure, complete with general anaesthetic. In fact, very similar to a colonoscopy.
NARRATION
An endoscope is first sent into the bowel to check the damage from the colitis.
Dr Alissa Walsh
So this here looks like a completely normal bowel. See all of the normal vessels? And then we get to the affected area here, which is about 15cm from the anus. And, as you can see, it's significantly different to what the normal bowel looks like.
Dr Graham Phillips
Yeah.
NARRATION
Those ulcers cause the terrible symptoms. After biopsies are taken, the team prepares for the faecal transplant.
Dr Alissa Walsh
The theory behind the faecal transplantation is that it's the ultimate probiotic. You're implanting live bacteria into another person's system to try to revert their flora to the flora of a patient without inflammatory bowel disease.
NARRATION
The faecal sample has to be placed far along the colon.
Dr Alissa Walsh
It's approximately a metre.
Dr Graham Phillips
Really?
Dr Alissa Walsh
Yeah, it's approximately a metre.
Dr Graham Phillips
It's a long way.
Dr Alissa Walsh
It's a long way. We find that putting it into this area helps the body to retain it better. This is the infusion going in now. She has three syringes, total of approximately 300ml.
NARRATION
The patient has several top-ups over the next two months. Then, they'll know if it's been successful.
Dr Graham Phillips
And did it work?
Anna Demasi
Yeah. Yeah, yeah, yeah. It worked. So I don't think I've ever gone to the shops so much before. You know, I can go for walks, I can play with my kid in the park, I don't have to sort of worry 'where's a toilet?', bring a change of clothes with me, all that sort of stuff.
NARRATION
We don't know yet if this works for everyone or even if it's a permanent cure, but if it does treat inflammatory bowel disease, the way is paved for other ailments, like emphysema and even multiple sclerosis.
Professor Sarkis K Mazmanian
In many ways, inflammatory bowel disease and multiple sclerosis are related on an immunologic level. The cells that attack the gut in inflammatory bowel disease are very similar to cells that attack the brain and the central nervous system in multiple sclerosis.
NARRATION
So Sarkis started experiments with mice.
Professor Sarkis K Mazmanian
Initially, we had shown that animals that had no gut bacteria did not develop multiple sclerosis. And so what this told us is that perhaps gut microbes had some role in triggering the inflammatory cascade that results in multiple sclerosis.
NARRATION
And the possibilities don't stop there. Sarkis has even found that autism seems to be related to gut bacteria.
Professor Sarkis K Mazmanian
Small molecules released by gut bacteria can travel through the circulation and potentially enter the brain and affect brain function.
NARRATION
Intriguingly, people with autism do often have gut problems and have different gut bacteria. And Sarkis's lab is working on a simpler treatment than a faecal transplant - a pill, developed from good bacteria, probiotics. And they've already treated autistic mice.
Professor Sarkis K Mazmanian
And the therapy that we used was a probiotic that our laboratory studied for many years that has effects, essentially, in repairing the gut. What we did was we administered this probiotic to animals that had autistic-like behaviour, and not only were we able to correct the gastrointestinal symptoms but we were able to also correct many of the behavioural symptoms that these mice exhibited, the behavioural symptoms that are associated with human autism.
NARRATION
It'll be some time before human trials can begin but, excitingly, other diseases may be treated by the same probiotic.
Professor Sarkis K Mazmanian
That is our long-term goal, is to potentially treat multiple sclerosis, inflammatory bowel disease, psoriasis, asthma, a variety of different autoimmune and allergic disorders, because the immune response that we believe triggers all of these disorders is very, very similar, and so the tissues may be different for these diseases, but the immune response is similar.
Gideon Cordover
I'm well into the second week now of my high-fibre diet. I'm so much better now. Last week, I was just complaining. I take it all back.
NARRATION
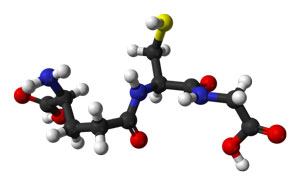
Researchers in Brisbane are working on a different pill to treat inflammatory disease. Matt Cooper's lab has studied the immune system receptor that vinegar locks into to work its magic. Now they're trying to improve on nature.
Professor Matt Cooper
We're looking at a different type of molecule that works on the same receptor, that does the same job but is more potent and lasts longer.
NARRATION
They design a molecule to latch onto the receptor.
Professor Matt Cooper
It's a bit like a key in the lock type of paradigm.
NARRATION
Then the molecule's churned out in bulk.
Dr Graham Phillips
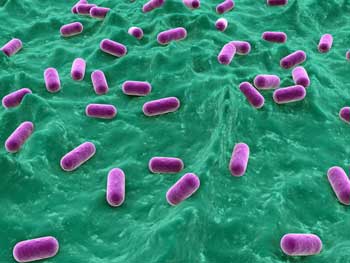
How do you produce large quantities of a single molecule that you've designed? Well, you trick a bacterium into doing it for you, with a bit of genetic tinkering. In this case, they're using E. coli, although a version of it that doesn't make you sick. You then multiply up the bacteria in a fermenter and collectively they produce grams of your designer compound.
NARRATION
The compound can't be used yet in people.
Professor Matt Cooper
What we can do is we can use animals as models for these diseases to try and help save human lives later. So we can induce a model of asthma and COPD in a mouse, and what's exciting, when we can stop all the effects of lung function, hypertension, all of the things that happen in the lung, we can ameliorate with the compound.
NARRATION
Human trials for this drug are about a decade away. Meanwhile, my gut results are in. The plots compare the types of bacteria I have with the general populations. Basically I've got a lot of Firmicutes and my overall profile is nowhere near typical.
Dr Graham Phillips
I seem to be quite far from normal in some areas. I don't know if that's good or bad.
Professor Rob Knight
Yeah, absolutely. So you were almost 100% Firmicutes, right?
Dr Graham Phillips
Yeah.
NARRATION
Alarmingly, Firmicutes often go hand in hand with obesity. But apparently I have a different kind.
Professor Rob Knight
So you've got a lot of Firmicutes, but what they are is mostly Ruminococcus, and so that's very interesting, because what the Ruminococcus is doing is it's tending to take your dietary fibre, and then it's fermenting that dietary fibre to butyrate in your large intestine. So do you also have a pretty high fibre intake?
Dr Graham Phillips
I do, yeah. This is sounding better. I was getting concerned that these were pretty bad bacteria.
Professor Rob Knight
No, absolutely not. Quite the contrary.
NARRATION
Rob can even tell some specifics.
Professor Rob Knight
It's interesting. We can make some guesses. So the Oxalobacter, that tends to show up if you eat a lot of leafy green vegetables, like silverbeet and things. Is that something that you do a lot of?
Dr Graham Phillips
Yeah, yeah, absolutely.
Professor Rob Knight
See, you're way out on the extremes for that...
NARRATION
So that was all good news for me. Those dairy and wheat intolerances seem to have done me a favour. But how would Gideon's gut bacteria be after his four-week high-fibre diet? Well, his results showed more good bacteria and a greater diversity. To see if that translated to better health, we gave him another fast food challenge and remeasured his bloods.
Dr Graham Phillips
So, you've got Gideon's new results. How did he go?
Professor Katherine Samaras
I do, and I want to know how you did it because the results are spectacular.
NARRATION
Gideon's blood sugars, fats and insulin response were vastly improved.
Professor Katherine Samaras
What was amazing for me was how much less insulin you needed. It took half the amount of insulin to clear the same amount of carbohydrate out of your system as it did the first time round. So everything is working so much better. How did you do it?
Gideon Cordover
Changed my diet. I replaced every bad meal that I used to be eating with good meals.
Dr Graham Phillips
I mean, that's pretty amazing, that just eating a good diet for one month has made all this difference.
Professor Katherine Samaras
The body senses food and responds to it almost immediately, so you can actually effect improvements in health within two or three days of changing your diet.
Dr Graham Phillips
So it's a pretty impressive result.
Gideon Cordover
It's good news, isn't it?
Dr Graham Phillips
Yeah.
Gideon Cordover
I can't believe it. I'm flabbergasted. It's great.
NARRATION
But can Gideon stick to the diet?
Dr Graham Phillips
So do you think you'll stick to it?
Gideon Cordover
It was relatively easy to get a really remarkable result and my insides are clearly much healthier now than they were before, so that's really inspired me to keep going, because if it is that easy, why not keep it up?
NARRATION
Using food as thy medicine is so simple yet so powerful... and open to all of us to put into practice.
http://www.med.monash.edu.au/cecs/gastro/prebiotic/resources/video-gallery.html
http://www.med.monash.edu.au/cecs/gastro/prebiotic/resources/menu-planning.html
NARRATION
New discoveries about food are rocking the foundations of medicine and nutrition.
Professor Charles Mackay
I think this is one of the biggest developments in medical research. I really think we're encountering a revolution that maybe we can prevent diseases by simply changing our diet.
NARRATION
Last time on Catalyst, we learned about this paradigm-changing new research.
Dr Graham Phillips
The bottom line is the modern Western diet could be making us very sick, contributing to heart disease, diabetes, asthma, emphysema, multiple sclerosis, even autism, and the list goes on.
NARRATION
The reason for the revelation that a good diet is even more important than we thought is the discovery of the many trillions of new contributors to our health - the tiny good bacteria living in our guts.
Professor Stephen Simpson
It's a jungle in there. So there's a whole series of really fascinating biological interactions.
NARRATION
In a nutshell, if you eat a bad diet, you end up with bad gut bacteria, and these bugs send the wrong messages to the immune system. You could wind up sick.
Dr Graham Phillips
Now it's all very well to know that the modern Western diet is causing health problems - but what do you do about it? Well, that's what this second episode is all about and I can tell you now it's more than just changing the food you eat.
NARRATION
The reason the modern diet is so unhealthy is it's drifted far from the diets we evolved to eat.
Professor Stephen Simpson
So, settled agriculture saw a massive change in our diet and then, clearly, since the industrialisation of agriculture and the industrialisation of our food processing.
NARRATION
Professor Steve Simpson's been catching this healthy, unprocessed, pre-agriculture food since he was a kid.
Dr Graham Phillips
If we were kind of living in the Stone Age days, this would be how we'd be catching a meal, apart from we wouldn't have the fishing rods.
Professor Stephen Simpson
We wouldn't.
Dr Graham Phillips
We'd have to catch it with our hands. Was there a Stone Age diet, a single diet?
Professor Stephen Simpson
I think there were many Stone Age diets. So if you were by the coast, like here, obviously fish and shellfish would've been a big part of the diet.
NARRATION
But while there was no one caveman diet, there was one thing all these diets had in common - a lot of fibre. We saw this in the last episode with Africa's Stone Age Hadza people.
Professor Stephen Simpson
An average person in the West, man or woman, is consuming less than 20g a day of dietary fibre. And to put that into an evolutionary perspective, six-month- to one-year-old Hadza kids are eating 50g to 200g of fibre a day, every day, and they do this throughout life.
NARRATION
Now to understand why fibre is so important, try to imagine the magical universe within.
Professor Stephen Simpson
In the gut what you have is essentially a container with an entire world inside of it comprising hundreds if not thousands of species.
NARRATION
Just as the many species in this mangrove live together in harmony as an ecosystem, so do the species in our intestines. The gut ecosystem is called the microbiome and, like any ecosystem, it's tipped out of balance if the creatures in it don't get one of their fundamental foods. And for the bugs living here that's fibre. That's why the low-fibre food we eat these days can be so damaging. To see the effects of that, in the last episode we met Gideon - a young, fit gymnast. The two of us took a junk food challenge. After a typical high-fat, high-sugar feed, we had our bloods measured to see the effects. And Gideon was shocked to learn that while he was fit on the outside, on the inside, my much older body was performing better than his.
Professor Katherine Samaras
And, Gideon, essentially you needed two to three times as much insulin.
Gideon Cordover
This is a huge shock to me and quite nerve-racking.
NARRATION
My insulin levels were considerably lower than Gideon's. Indeed, he was on the road to diabetes. Why would this much younger man have such an unhealthy response? It became clear when we looked in his fridge. Not many health foods here.
Gideon Cordover
So I wake up in the morning, often I will eat what we had for dinner last night, tends to be kind of fast foods, so sometimes that'll be pizza. I'm a big fan of chicken burgers, so I eat a lot of fast food meals which often come with French fries, so big fan of French fries as well. Occasionally I eat at the pub - it will be usually a chicken burger, fries.
NARRATION
Almost all of Gideon's diet is processed food.
Professor Katherine Samaras
When we eat processed foods, it generates a whole lot of bacteria in our body that promotes inflammation, and these are the bad bacteria.
NARRATION
But the good news is give up the junk food and the inflammation reaction is turned down.
Professor Katherine Samaras
People who are lean and eat unprocessed food regularly have got all the good bacteria in their intestines.
NARRATION
So, we put a proposal to Gideon.
Dr Graham Phillips
Well, have we got an offer for you! How would you like us to put you on a healthy diet and see what changes it makes to your gut bacteria?
Gideon Cordover
A healthy diet?
Dr Graham Phillips
Carrot sticks, you know...
Gideon Cordover
A tasty diet?
Dr Graham Phillips
A tasty diet. It will be designed by a dietician.
Gideon Cordover
OK.
NARRATION
Monash University nutrition researcher Trish Veitch cooked up four weeks of healthy meals for Gideon.
Gideon Cordover
I'm nervous that I won't like the taste of some of the food that I'm gonna be eating, and I'm a bit nervous that I will feel hungry all the time because I'm used to eating huge quantities of fast food.
NARRATION
She also took him shopping, showing him the kind of food he should be buying.
Trish Veitch
These are persimmons. They're a source of really good prebiotic fibre.
Gideon Cordover
A whole new world of fruit and veg.
Trish Veitch
Indeed.
Gideon Cordover
The doctor said that this isn't, kind of, permanent damage that's been done, and so I guess it's given me more impetus to really take this diet seriously and actually make a good go of it.
Trish Veitch
Any of these beans are good for you.
Gideon Cordover
OK.
NARRATION
The plan is we'll look at Gideon's gut bacteria before and after his new diet, and we'll also remeasure his insulin response after four weeks of eating this healthy, but most importantly, high-fibre food.
Trish Veitch
Terrific.
Dr Graham Phillips
Alright. Yes, I reckon... can you do those zucchinis in thin strips?
NARRATION
Now, as it happens, I've been eating a fairly high-fibre diet lately.
Dr Graham Phillips
Yeah, that's perfect.
NARRATION
It wasn't my choice. Rather, I've developed allergies to dairy and wheat products - they give me sinus problems. And when you cut those out, you're left eating fairly high-fibre food.
Dr Graham Phillips
Now I eat about 50g of fibre a day, which is more than twice as much as the average Australian. I wonder what effect that's having on my gut bacteria.
NARRATION
Well, there's a way to find out. In Boulder, Colorado, is the headquarters of the American Gut Project. Here they collect samples of people's faeces from around the world, examining them to see just what kind of gut bacteria we're all carrying. Why are they doing it? I Skyped Rob Knight to find out.
Dr Graham Phillips
G'day, Rob.
Professor Rob Knight
Hey, Graham.
Dr Graham Phillips
What's the purpose of it? Why are you doing it?
Professor Rob Knight
Well, we're trying to find out what kinds of microbiomes are out there in the world. We're just beginning to find out how many kinds of communities there are even on one person.
NARRATION
By looking at samples from a wide variety of people, the goal is to eventually match particular microbiomes with particular health problems. Donating to the program is as simple as asking for a kit, and it can be fun.
Professor Rob Knight
You can also give it a gift to someone else, right? So if you have some family member, OK, you've just been dying all along to figure out exactly what kind of shit they're full of, now you can do that.
Dr Graham Phillips
Well, look, I always like to donate to worthy causes. This is kind of a bit odd, this one. But you'd accept a donation from me?
Professor Rob Knight
Absolutely.
NARRATION
Three days later, the kit turned up in the mail.
Dr Graham Phillips
Instructions. 'Collect a small amount of... biomass.' Way of putting it. 'More is not better.' OK. The things I do for science. But I guess it will be good to know what kind of gut bacteria I have.
Gideon Cordover
Hello, and welcome to day one of my video diary. For dinner, brown rice with lentils, which was a shock. And I had Greek yoghurt, Ryvita with hummus. Heaps and heaps of nuts. All kinds of nuts. Almonds and pistachios. I have experienced some mild discomfort, I would have to say, in terms of the old abdominal bloating.
NARRATION
Now, eating more fibre will improve your health. But there are other things you might be able to do, as well.
Dr Graham Phillips
Cheers.
Professor Matt Cooper
Cheers. That's quite sweet.
Dr Graham Phillips
Yeah. That's not bad.
Professor Matt Cooper
Shall we do shots?
Dr Graham Phillips
Shots sound perfect.
Professor Matt Cooper
Shots it is.
Dr Graham Phillips
Cheers.
Professor Matt Cooper
Down the hatch.
Dr Graham Phillips
Hoo!
Professor Matt Cooper
Ahh!
Dr Graham Phillips
Not as sweet. Ah!
NARRATION
This is no social drink. Professor Matt Cooper and I may be medicating ourselves. But they won't be adding these tipples to the wine list anytime soon. We're downing different kinds of vinegar because it could turn out to be a medicine.
Professor Matt Cooper
So the most important thing is to have a balanced diet and lots of high fibre. But we've also shown that with a lot of the studies we're doing in animals now that supplementing the diet by giving vinegar can actually stop things like asthma.
NARRATION
Treating asthma with vinegar? It seems remarkable. Unless of course you're into alternative health.
Dr Graham Phillips
The idea of using vinegar medicinally has been around for centuries.
Professor Matt Cooper
Oh, thousands of years, back to the Egyptian times, the Greek times. The beneficial effects of vinegars in society have been known for a long time. Even Italians - a lot of vinegar on salads, a lot of vinaigrette - they have very, very low incidences of inflammatory disease.
NARRATION
In fact, even the research on eating a good diet has an air of ancient wisdom about it.
Professor Charles Mackay
Hippocrates said 'Let thy food be thy medicine and thy medicine be thy food.' And we agree with that entirely.
NARRATION
The reason vinegar could be a medicine is because it contains acetate - that molecule we met in the first episode, the very one our good bacteria make.
Professor Matt Cooper
So we now know that acetate, which is very small and can get all around the body, can stop the immune system from overreacting.
NARRATION
By calming the immune system, it promotes good health. Matt Cooper developed asthma at about 18.
Professor Matt Cooper
I ended up taking a puffer twice a day and I was taking steroids two or three times a day. I had several incidents where I was really worried, I was almost gonna go to hospital, it was that bad. I was taking puff after puff, I could barely breathe.
Alessio
It hurts your chest a lot when you cough.
NARRATION
But now he's started eating more fibre and using liberal quantities of vinegar.
Professor Matt Cooper
I radically changed my diet. I dropped certain processed foods, I made sure it was brown rice, brown pasta, brown bread, bran in the morning and lots of fresh fruit and vegetables. And now I probably have one puff a year, if that.
Dr Graham Phillips
Really?
Professor Matt Cooper
Yeah.
Gideon Cordover
It's kind of going OK. I miss fast food. I really miss it.
NARRATION
Now, there are no proper clinical trials yet proving that vinegar can treat asthma in people, but there are results for mice. After showing she could reduce asthma in these animals by simply feeding them high-fibre food, Alison tried something else - she fed them acetate instead.
Dr Alison Thorburn
In fact, when we give acetate directly in the drinking water to the mice, that also suppressed their asthma.
NARRATION
So it seems incredible that simple stuff we splash on a salad may help treat a disease that plagues the Western world. And Alison's asthma story has taken yet another twist. She's fed high fibre to pregnant mice.
Dr Graham Phillips
Ah, there she is. So she's just given birth, has she?
Dr Alison Thorburn
Yeah, so she just gave birth yesterday morning.
Dr Graham Phillips
And so you've found something special about the diet in pregnant mice, right?
Dr Alison Thorburn
That's right. So she was actually on a high-fibre diet, and what we found was that when we gave pregnant mice the high-fibre diet and had a look at their offspring, their offspring didn't develop asthma. So they were protected against the development of asthma.
Dr Graham Phillips
So this is another thing for poor old mothers, is it? They can't drink, they can't smoke.
Dr Alison Thorburn
That's right.
Dr Graham Phillips
They've got to eat a high-fibre diet to reduce asthma.
Dr Alison Thorburn
Yep, yep.
NARRATION
Gut bacteria are tied up with a lot of other diseases, too. Take Professor Phil Hansbro's research on the devastating lung disease emphysema.
Professor Phil Hansbro
There are no current treatments that effectively suppress the disease and there's no treatments that stop the progression of disease.
NARRATION
Emphysema is a form of chronic obstructive pulmonary disorder, COPD.
Professor Phil Hansbro
A good way of explaining COPD is like taking a deep breath and then trying to take in a bit more breath and that last bit is the only breath that people with COPD can breathe in.
Dr Graham Phillips
Really? Let me try that. (Inhales deeply)
Professor Phil Hansbro
So another way of explaining it...
Dr Graham Phillips
Yeah, that's pretty awful.
Professor Phil Hansbro
Another way of explaining it is like trying to breathe through a straw.
NARRATION
The leading cause of emphysema in Australia is smoking. And remarkably, this activity, in mice at least, can push the gut microbiome out of balance.
Professor Phil Hansbro
So we think it not just affects the lung but there's systemic effects, and so that it affects the microbiome in the gut. We can show the changes in the microbiome that occur with cigarette smoke exposure and then we can also show which bacteria are altered, so which ones increase and which ones decrease.
NARRATION
And, excitingly, Phil's also found it may be possible to switch a bad emphysema biome for a more healthy one.
Professor Phil Hansbro
So mice are very good animals to study for this disease because when you co-house them they are actually coprophiles, and so they eat each other's poo.
NARRATION
Poo contains gut bacteria. Eat another's, and one acquires their bacteria.
Professor Phil Hansbro
So you can put mice in a box, some that are healthy and some that have COPD and emphysema, and they'd swap their microbiomes through eating each other's poo.
NARRATION
And the incredible result is mice that have emphysema get an improvement in symptoms after eating the poo of healthy mice. New gut bacteria have treated them.
Professor Phil Hansbro
It's really exciting stuff.
Dr Graham Phillips
So the good news is you've found a potential treatment for emphysema. The bad news is we have to eat each other's poo.
Professor Phil Hansbro
Well, that's quite correct. Although we can make it a lot more palatable by... and we call this 'transpoosion', which is a term that we're trying to bring into the literature.
NARRATION
Phil's transpoosion is, yep, a poo transplant. It involves taking faeces from a healthy person and putting them in the gut of someone suffering disease - hence providing them with new gut bacteria. Officially, it's known as a faecal transplant.
Dr Graham Phillips
I must say, this is one of the strangest procedures I've filmed as a science journalist. And, hey, I once filmed myself drinking my own urine, which I'd like to point out was properly filtered beforehand. But, you know, we may snigger and be a bit revolted by this procedure, but it could turn out to be a really important treatment.
NARRATION
No-one is yet doing faecal transplants in people for emphysema. But they are trialling the procedure for another debilitating disease thought to be connected to bad gut bacteria - ulcerative colitis. It's an inflammatory bowel disease and Anna has suffered it for more than half a decade.
Anna Demasi
So I was sick at about 22, so I'm 29 now, and I had really bad diarrhoea, you know, I couldn't control it, going to the toilet, you know, 30, 40 times a day. And I couldn't sleep, fevers, sore back. Those 30, 40 times a day was not food, it was mostly just blood and water.
Dr Graham Phillips
I mean, that must have had a huge impact on your life.
Anna Demasi
You can't go anywhere. You can't plan for trips, can't plan anything, can't even go to the shops to buy something.
NARRATION
This inflammatory bowel disease can be treated with powerful drugs but they can have terrible side effects.
Anna Demasi
My face would blow up like three times the size in a matter of days. I'd put 10, 15 kilos in a matter of a few weeks. And then the mental things, you'd get quite anxious and very aggressive. And you also couldn't sleep at night. So just a horrible, really horrible drug.
NARRATION
So a new treatment for the condition is being trialled at Sydney's St Vincent's Hospital - a faecal transplant.
Dr Graham Phillips
Now, it's a full medical procedure, complete with general anaesthetic. In fact, very similar to a colonoscopy.
NARRATION
An endoscope is first sent into the bowel to check the damage from the colitis.
Dr Alissa Walsh
So this here looks like a completely normal bowel. See all of the normal vessels? And then we get to the affected area here, which is about 15cm from the anus. And, as you can see, it's significantly different to what the normal bowel looks like.
Dr Graham Phillips
Yeah.
NARRATION
Those ulcers cause the terrible symptoms. After biopsies are taken, the team prepares for the faecal transplant.
Dr Alissa Walsh
The theory behind the faecal transplantation is that it's the ultimate probiotic. You're implanting live bacteria into another person's system to try to revert their flora to the flora of a patient without inflammatory bowel disease.
NARRATION
The faecal sample has to be placed far along the colon.
Dr Alissa Walsh
It's approximately a metre.
Dr Graham Phillips
Really?
Dr Alissa Walsh
Yeah, it's approximately a metre.
Dr Graham Phillips
It's a long way.
Dr Alissa Walsh
It's a long way. We find that putting it into this area helps the body to retain it better. This is the infusion going in now. She has three syringes, total of approximately 300ml.
NARRATION
The patient has several top-ups over the next two months. Then, they'll know if it's been successful.
Dr Graham Phillips
And did it work?
Anna Demasi
Yeah. Yeah, yeah, yeah. It worked. So I don't think I've ever gone to the shops so much before. You know, I can go for walks, I can play with my kid in the park, I don't have to sort of worry 'where's a toilet?', bring a change of clothes with me, all that sort of stuff.
NARRATION
We don't know yet if this works for everyone or even if it's a permanent cure, but if it does treat inflammatory bowel disease, the way is paved for other ailments, like emphysema and even multiple sclerosis.
Professor Sarkis K Mazmanian
In many ways, inflammatory bowel disease and multiple sclerosis are related on an immunologic level. The cells that attack the gut in inflammatory bowel disease are very similar to cells that attack the brain and the central nervous system in multiple sclerosis.
NARRATION
So Sarkis started experiments with mice.
Professor Sarkis K Mazmanian
Initially, we had shown that animals that had no gut bacteria did not develop multiple sclerosis. And so what this told us is that perhaps gut microbes had some role in triggering the inflammatory cascade that results in multiple sclerosis.
NARRATION
And the possibilities don't stop there. Sarkis has even found that autism seems to be related to gut bacteria.
Professor Sarkis K Mazmanian
Small molecules released by gut bacteria can travel through the circulation and potentially enter the brain and affect brain function.
NARRATION
Intriguingly, people with autism do often have gut problems and have different gut bacteria. And Sarkis's lab is working on a simpler treatment than a faecal transplant - a pill, developed from good bacteria, probiotics. And they've already treated autistic mice.
Professor Sarkis K Mazmanian
And the therapy that we used was a probiotic that our laboratory studied for many years that has effects, essentially, in repairing the gut. What we did was we administered this probiotic to animals that had autistic-like behaviour, and not only were we able to correct the gastrointestinal symptoms but we were able to also correct many of the behavioural symptoms that these mice exhibited, the behavioural symptoms that are associated with human autism.
NARRATION
It'll be some time before human trials can begin but, excitingly, other diseases may be treated by the same probiotic.
Professor Sarkis K Mazmanian
That is our long-term goal, is to potentially treat multiple sclerosis, inflammatory bowel disease, psoriasis, asthma, a variety of different autoimmune and allergic disorders, because the immune response that we believe triggers all of these disorders is very, very similar, and so the tissues may be different for these diseases, but the immune response is similar.
Gideon Cordover
I'm well into the second week now of my high-fibre diet. I'm so much better now. Last week, I was just complaining. I take it all back.
NARRATION
Researchers in Brisbane are working on a different pill to treat inflammatory disease. Matt Cooper's lab has studied the immune system receptor that vinegar locks into to work its magic. Now they're trying to improve on nature.
Professor Matt Cooper
We're looking at a different type of molecule that works on the same receptor, that does the same job but is more potent and lasts longer.
NARRATION
They design a molecule to latch onto the receptor.
Professor Matt Cooper
It's a bit like a key in the lock type of paradigm.
NARRATION
Then the molecule's churned out in bulk.
Dr Graham Phillips
How do you produce large quantities of a single molecule that you've designed? Well, you trick a bacterium into doing it for you, with a bit of genetic tinkering. In this case, they're using E. coli, although a version of it that doesn't make you sick. You then multiply up the bacteria in a fermenter and collectively they produce grams of your designer compound.
NARRATION
The compound can't be used yet in people.
Professor Matt Cooper
What we can do is we can use animals as models for these diseases to try and help save human lives later. So we can induce a model of asthma and COPD in a mouse, and what's exciting, when we can stop all the effects of lung function, hypertension, all of the things that happen in the lung, we can ameliorate with the compound.
NARRATION
Human trials for this drug are about a decade away. Meanwhile, my gut results are in. The plots compare the types of bacteria I have with the general populations. Basically I've got a lot of Firmicutes and my overall profile is nowhere near typical.
Dr Graham Phillips
I seem to be quite far from normal in some areas. I don't know if that's good or bad.
Professor Rob Knight
Yeah, absolutely. So you were almost 100% Firmicutes, right?
Dr Graham Phillips
Yeah.
NARRATION
Alarmingly, Firmicutes often go hand in hand with obesity. But apparently I have a different kind.
Professor Rob Knight
So you've got a lot of Firmicutes, but what they are is mostly Ruminococcus, and so that's very interesting, because what the Ruminococcus is doing is it's tending to take your dietary fibre, and then it's fermenting that dietary fibre to butyrate in your large intestine. So do you also have a pretty high fibre intake?
Dr Graham Phillips
I do, yeah. This is sounding better. I was getting concerned that these were pretty bad bacteria.
Professor Rob Knight
No, absolutely not. Quite the contrary.
NARRATION
Rob can even tell some specifics.
Professor Rob Knight
It's interesting. We can make some guesses. So the Oxalobacter, that tends to show up if you eat a lot of leafy green vegetables, like silverbeet and things. Is that something that you do a lot of?
Dr Graham Phillips
Yeah, yeah, absolutely.
Professor Rob Knight
See, you're way out on the extremes for that...
NARRATION
So that was all good news for me. Those dairy and wheat intolerances seem to have done me a favour. But how would Gideon's gut bacteria be after his four-week high-fibre diet? Well, his results showed more good bacteria and a greater diversity. To see if that translated to better health, we gave him another fast food challenge and remeasured his bloods.
Dr Graham Phillips
So, you've got Gideon's new results. How did he go?
Professor Katherine Samaras
I do, and I want to know how you did it because the results are spectacular.
NARRATION
Gideon's blood sugars, fats and insulin response were vastly improved.
Professor Katherine Samaras
What was amazing for me was how much less insulin you needed. It took half the amount of insulin to clear the same amount of carbohydrate out of your system as it did the first time round. So everything is working so much better. How did you do it?
Gideon Cordover
Changed my diet. I replaced every bad meal that I used to be eating with good meals.
Dr Graham Phillips
I mean, that's pretty amazing, that just eating a good diet for one month has made all this difference.
Professor Katherine Samaras
The body senses food and responds to it almost immediately, so you can actually effect improvements in health within two or three days of changing your diet.
Dr Graham Phillips
So it's a pretty impressive result.
Gideon Cordover
It's good news, isn't it?
Dr Graham Phillips
Yeah.
Gideon Cordover
I can't believe it. I'm flabbergasted. It's great.
NARRATION
But can Gideon stick to the diet?
Dr Graham Phillips
So do you think you'll stick to it?
Gideon Cordover
It was relatively easy to get a really remarkable result and my insides are clearly much healthier now than they were before, so that's really inspired me to keep going, because if it is that easy, why not keep it up?
NARRATION
Using food as thy medicine is so simple yet so powerful... and open to all of us to put into practice.
- Reporter: Dr Graham Philips
- Producer: Geraldine McKenna, Co-Producer: Roslyn Lawrence
- Researcher: Roslyn Lawrence
- Camera: Nick Castellaro
David Collins
Tony Connors
Ron Ekkel
Simon Green
Phil Hankin
Zumi Hidalgo
Andrew McClymont
Campbell Miller
Larry Neukum
Daniel Shaw
Additional cameras:
High Speed Camera – Tony Connors
Roslyn Lawrence - Sound: Chris Coltman
Graham Fettling
James Fisher
Paul Freeman
Chris Gillette
Martin Harrington
Gavin Marsh
Tim Parratt - Editor: Vaughan Smith
STORY CONTACTS
Prof Rob Knight
BioFrontiers Institute
University of Colorado, Boulder
BioFrontiers Institute
University of Colorado, Boulder
Professor Stephen Simpson
Charles Perkins Centre
Uni of Sydney
Charles Perkins Centre
Uni of Sydney
Professor Charles Mackay
School of Biomedical Sciences
Monash University
School of Biomedical Sciences
Monash University
Prof Sarkis K. Mazmanian
Biology and Biological Engineering
California Institute of Technology
Biology and Biological Engineering
California Institute of Technology
Prof Matt Cooper
Institute for Molecular Bioscience
University of Queensland
Institute for Molecular Bioscience
University of Queensland
Dr Jeff Leach
Founder
Human Food Project
Founder
Human Food Project
Dr Alison Thorburn
School of Biomedical Sciences
Monash University
School of Biomedical Sciences
Monash University
Prof Katherine Samaras
Endocrinologist
St Vincent's Hospital, Darlinghurst
Endocrinologist
St Vincent's Hospital, Darlinghurst
Prof Phil Hansbro
RELATED INFO
READING
Sarkis Mazmanian’s paper on probiotic and neurodevelopment disorders
http://www.cell.com/abstract/S0092-8674(13)01473-6
http://www.cell.com/abstract/S0092-8674(13)01473-6
Rob Knight’s paper on diversity, resilience and stability in the gut microbiota
http://www.ncbi.nlm.nih.gov/pubmed/22972295
http://www.ncbi.nlm.nih.gov/pubmed/22972295